Georgia Tech engineers have determined that the manipulation of cells by a new microfluidic device may help clinicians improve a promising cancer therapy that harnesses the body's own immune cells to fight such diseases as metastatic melanoma, non-Hodgkin's lymphoma, chronic lymphocytic leukemia and neuroblastoma.
The therapy, known as adoptive T cell transfer, has shown encouraging results in clinical trials. This treatment involves removing disease-fighting immune cells called T cells from a cancer patient, multiplying them in the laboratory and then infusing them back into the patient's body to attack the cancer. The effectiveness of this therapy, however, is limited by the finite lifespan of T cells -- after many divisions, these cells become unresponsive and inactive.
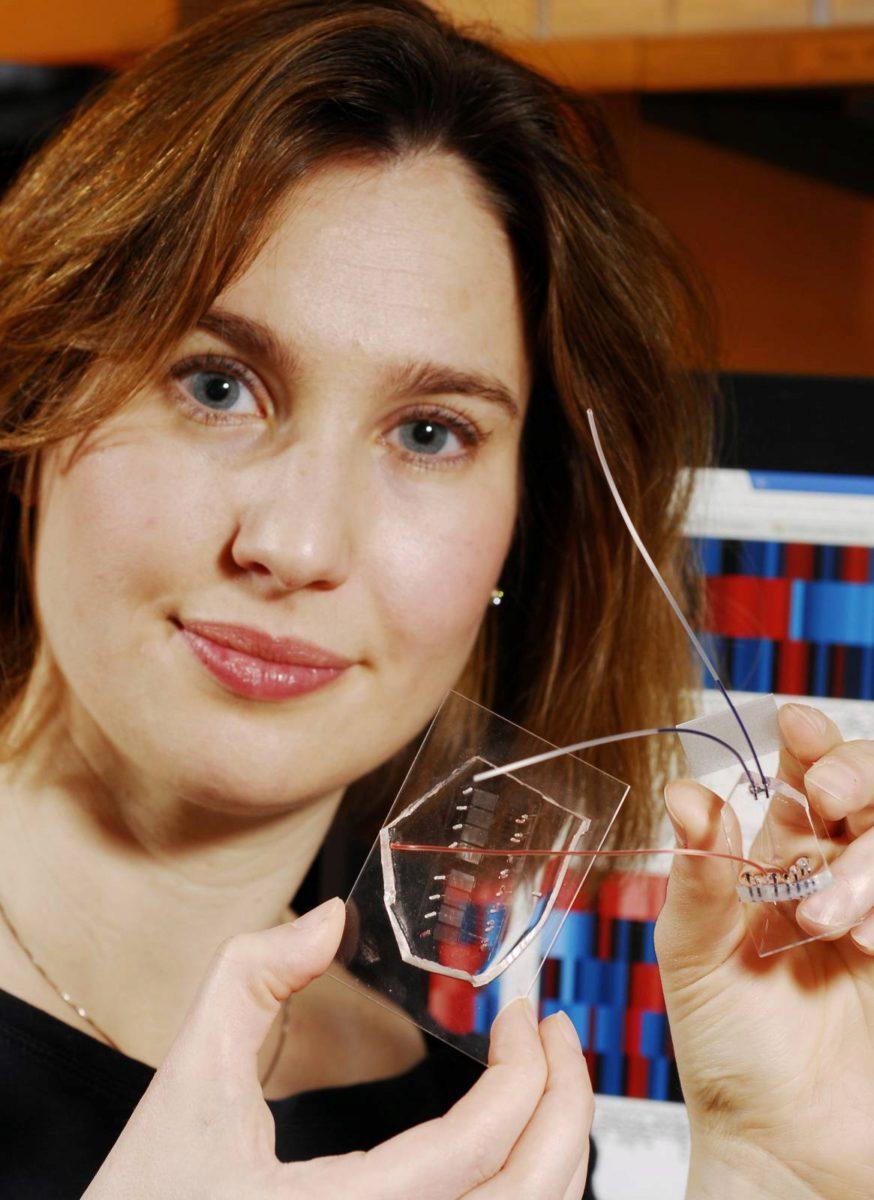
Researchers at Georgia Tech and Emory University have addressed this limitation by developing a microfluidic device for sample handling that allows a statistical model to be generated to evaluate cell responsiveness and accurately predict cell "age" and quality. Being able to assess the age and responsiveness of T cells -- and therefore transfer only young functional cells back into a cancer patient's body -- offers the potential to improve the therapeutic outcome of several cancers.
"The statistical model, enabled by the data generated with the microfluidic device, revealed an optimal combination of extracellular and intracellular proteins that accurately predict T cell age," said Melissa Kemp, an assistant professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. "Knowing this information will help facilitate the clinical development of appropriate T cell expansion and selection protocols."
With the donor T cell data, the researchers developed a model to assess which biomarkers or dynamical signaling events best predicted the quality of T cell function. The model found the most informative data in predicting cellular age to be the initial changes in signaling dynamics. "Although a combination of biomarker and dynamic signaling data provided the optimal model, our results suggest that signaling information alone can predict cellular age almost as well as the entire dataset," noted Kemp. In the future, Kemp plans to use this approach of combining multiple cell-based experiments on a microfluidic chip to integrate single-cell information with population-averaged techniques, such as multiplexed immunoassays or mass spectrometry.