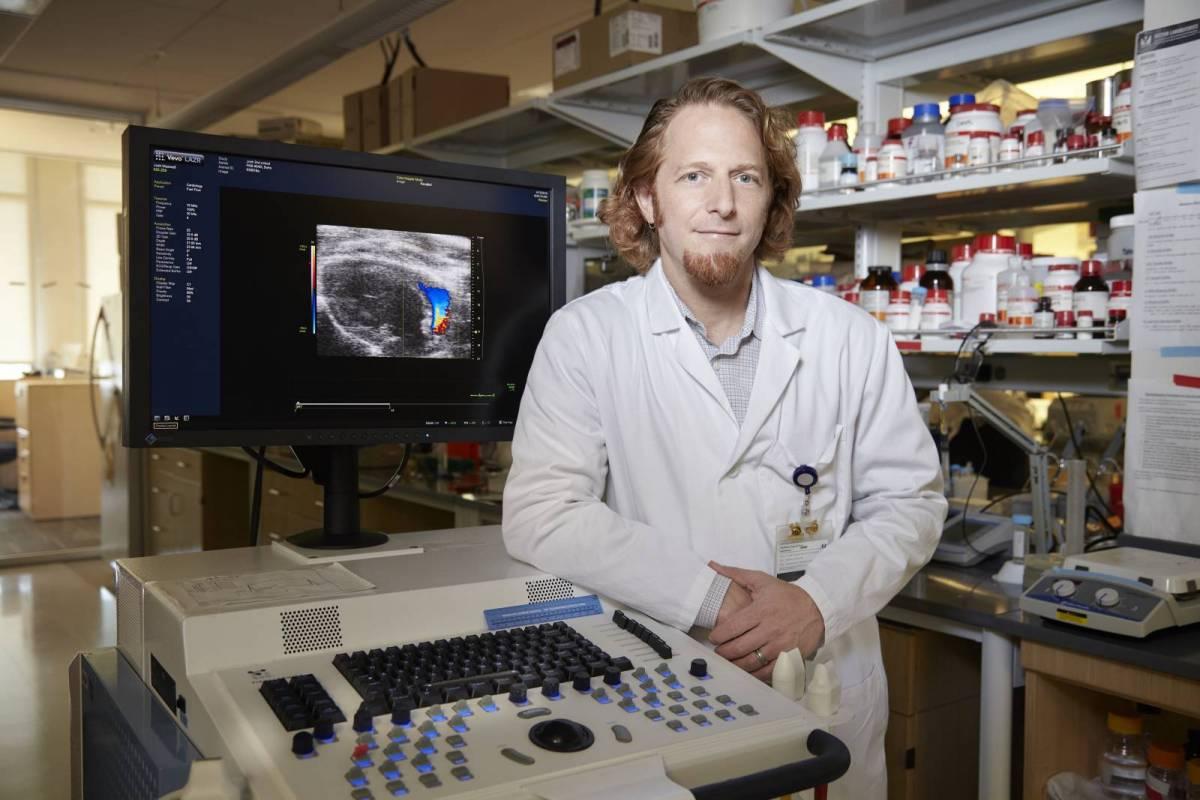
Michael Davis changes the landscape of pediatric cardiology with stem cell therapies and 3D printing

Congenital heart disease (CHD) affects nearly nine in every 1,000 babies born. In fact, it’s the world’s most common birth defect. Researchers and clinicians today have begun applying stem cell therapies and 3D tissue printing to pediatric heart defects. Michael Davis, director of Children’s Healthcare of Atlanta's Heart Research and Outcomes Center (HeRO) under the Georgia Tech and Emory University’s Department of Biomedical Engineering, is busy pushing the boundaries on innovative stem cell research with clinical trials, predictive medicine models and 3D printing.
Davis’ lab focuses on pediatric heart failure and general defects. Mostly, he’s dealing with patients who have congenital issues, including hypoplastic left heart syndrome (HLHS) and left ventricular cardiomyopathy. Being local to Atlanta, Children’s Healthcare of Atlanta offers Davis and his team of researchers access to a large volume of young cardiac patients who need the help of his new and developing therapies.
“With pediatrics, clinicians are very open to collaborating and trying new procedures and therapies,” said Davis. “In the pediatric world, there are fewer options for these kids, and the parents and clinicians are hungry for new therapies to try.”

Designing Targeted Stem Cell Therapies
A few years ago, Davis noticed that during bypass surgery, small amounts of tissue were being removed to run the bypass tubing into the heart, and surgeons were throwing it away after removal. As the new director of HeRO at the time, he asked and was granted permission to use the tissue in his research lab for stem cell studies. Davis began extracting and quantifying the stem cells, eventually finding that the young cells had more reparative qualities, and when injected into damaged tissue, released healing proteins.
Davis’ first clinical trial with the stem cells (Autologous Cardiac Stem Cell Injection in Patients with Hypoplastic Left Heart Syndrome (ACT-HLHS) Trial) is happening in the next few months and has already been cleared by the FDA. Clinicians will inject the stem cells into the hearts of babies with CHD to boost the function of the heart.
“For a baby with HLHS, we are not going to re-grow the left ventricle, but rather try to strengthen and prevent deterioration of the existing right ventricle,” said Davis. “It sets the baby up for a successful repair surgery down the road.”
In his lab, Davis observes the cells and gathers quantitative data on their behavior. The research is conducted for cord blood, bone marrow and cardiac stem cells, which is where Davis’ work is revolutionizing his field. Davis and Manu Platt, diversity director of STC on Emergent Behaviors of Integrated Cellular Systems (EBICS) at Georgia Tech, have written a grant in the hopes of combining all the cellular data from patients in three different clinical trials to create a large data repository of cell signals. By studying the signals, otherwise known as protein secretions of the cell, Davis and Platt can determine how effective certain cells are in treating diseases.
“These cells could be acting a number of ways, and we want to collect all the information we can, including their genome and what they release,” said Davis. “We essentially want to make equations to determine how cells will respond. We want to put the data together to create a treatment prediction.”
With this information, they will be able to build a mathematical model that identifies the cell genome in order to predict what the cell will do in the clinic. The goal is to identify the best characteristics of these cells and determine which diseases they can target to begin the reparative process.
“If we can study the cells and isolate their response, we will be able to provide personalized approaches to stem cell therapy – that’s really what the field is currently lacking,” said Davis. “A patient could come in, and we could sequence their cells and know immediately what cells to inject for the best outcome. Different cells are going to have differing effects on each individual.”

Innovations in 3D Printing
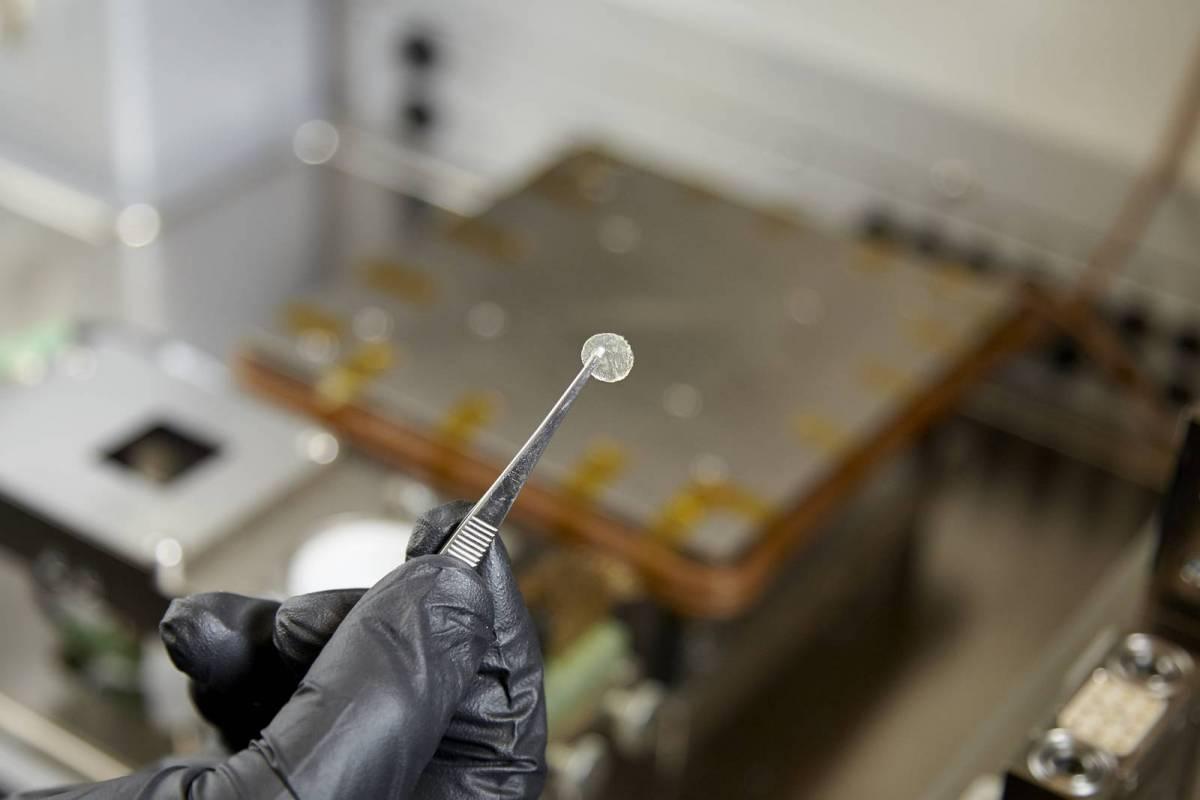
The 3D printing in Davis’ lab is used to create valves, leaflets and patches. Aline Nachlas, a fourth-year PhD biomedical engineering candidate, has earned a fellowship for tissue engineering, with the goal of creating valve cells. She has also found a material that will support the printing of these cells. The valves are made using skin cells from the patient, so essentially, they are growing their own cells, minimizing the risk of organ rejection. And ideally, the valve will continue to grow with the patient, never needing to be replaced.
“We hope these cells will be able to print valves, or at least the leaflets that make up valves,” said Davis. “Currently, children are undergoing animal valve replacements, which are sometimes too big, and they don’t grow with the child. This means more surgeries down the road to replace the valve, as well as high doses of immunosuppressants. We want to create a living valve that grows with the child.”
Davis’ lab is also working on a printable patch that contains stem cells. The patch functions to keep all the stem cells in one place, so the cells can repair the surrounding tissue. Davis’ student is hoping to print the patch scaffold with a decellularized pig material matrix.
“Very few people are trying to heal with 3D printed patches,” said Davis. “My lab is on the forefront of that research. We are trying to make a positive contribution in a sensible way.”
Next up for Davis is a summer trip to Galway, an international biotechnology hub, where he will teach tissue engineering to Georgia Tech biomedical engineering students. In the next five to 10 years, he hopes to be more focused on 3D printing and really pushing the envelope on printing small tissues. Davis wants to bring more regenerative therapies to the greatest number of children possible.
“My research may not always move at the speed I want, so I try to remember there is a bigger picture,” said Davis. “We are already helping many kids with CHD become healthier and stronger. But, I am always asking myself ‘what can we do better?’”