These engineers approach robotics from different angles, but they share the same goal - they want to develop wearable robotic devices that can help people maintain or increase their mobility.
Aaron Young and Greg Sawicki's labs in Georgia Tech’s George W. Woodruff School of Mechanical Engineering are laying the groundwork for a range of devices that could help children, stroke patients, the elderly, and amputees gain more independence and move with greater comfort and ease.
“My goal in the lab is to make sure that people can do what they want to do as long as they want to,” says Sawicki. “That might be a big challenge, but it’s a straightforward guiding principle- make people happy by allowing them to keep moving.”
Aaron Young approaches these challenges as a controls specialist focused on how the human body can interface with a robotic device. The human body processes countless signals every time a person moves, so he is focused on translating those neural signals into commands for a range of exoskeletons and prostheses that can perform as seamlessly as if they were a part of the body.
"I was always really interested on the control side of things, understanding how to take biological signals or neural signals from the human and use that to control robotic devices," says Young. "That was really my focus as a graduate student at Northwestern and what got me into this field of human augmentation and assistive restoration with prostheses and exoskeletons."
"I'm trying to understand how to unite the human user with their assistive robotic technology. A major part of that focus is on something that we call intent recognition which is really trying to understand what a person is trying to do and then use different artificial intelligence and machine learning techniques to take sensor information from the human and the robot and use that to appropriately give assistance."
With Young focused on the human-machine interface and control systems, Sawicki looks at the neuromechanics and energetics of human locomotion and how movement can be augmented with wearable technology. An avid runner and biker, he has always been fascinated with the efficiency of movement, and he is focused on finding ways to restore that efficiency to people who are lacking in it. If that can be done, they could live more active lifestyles over a longer period of time. Sawicki also looks at the impact wearable devices have on the body itself, whether that’s in terms of energy cost or how something attached to a person’s ankle might impact their knee or hip.
As he puts it, “When I got involved with wearable robotics I saw that we're attaching something to the outside of a very complex structure- the human body. And if you don't think at all about what's happening under the skin you're not going to solve the problem. You have to understand muscles and how they work to build good robots.”
And make no mistake- Sawicki and Young are building good robots, even though they might not be what comes to mind when most people think of robots.
Their devices are wearable, and have varying degrees of electronics and coding built into them. Though the technology behind them varies, they all share a common goal- to make it easier for people to be mobile. Here are some of the projects they are working on.

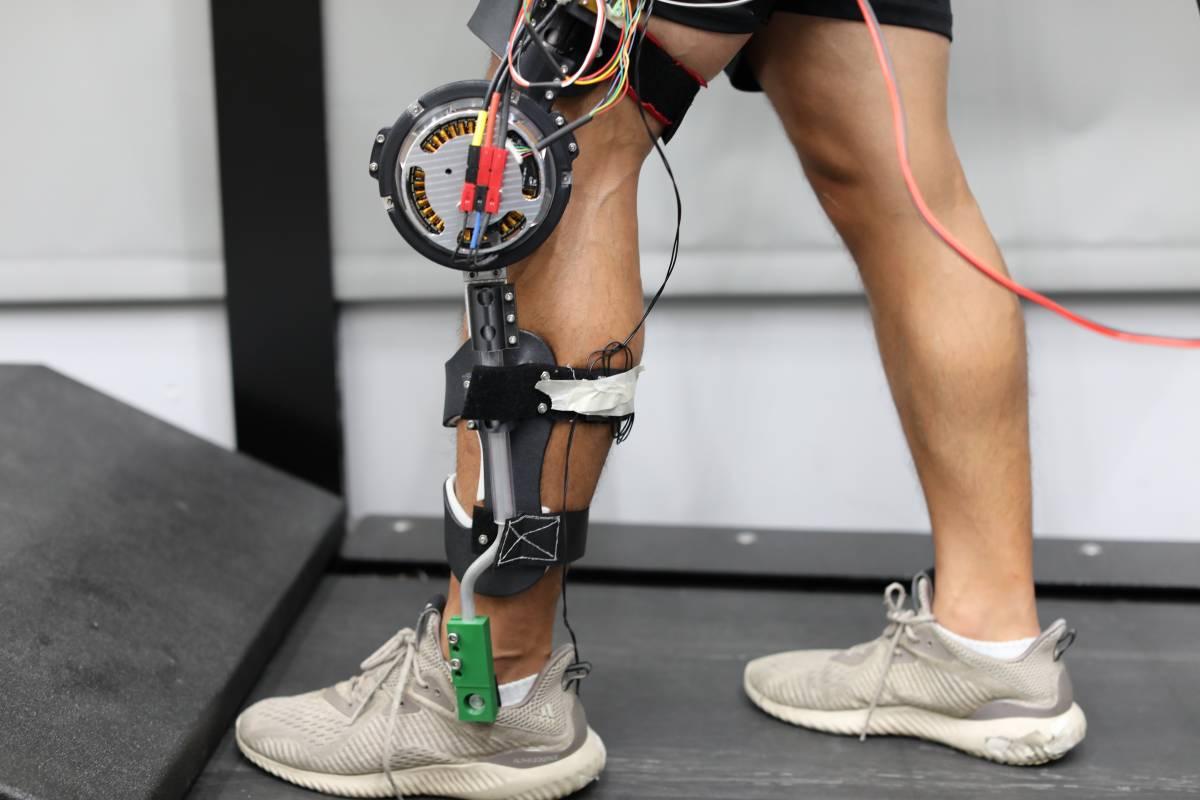
Knee Exoskeleton
Young is developing a lightweight low-profile knee exoskeleton for children with cerebral palsy that helps them counteract a condition known as crouch gait. The condition is caused by perpetually tense muscles and tendons, and the knee exoskeleton is being designed to act as a mechanical intervention that helps retrain the tendons, muscles, and the brain by reinforcing a more biomechanically efficient gait. Right now treatment options include physical therapy and surgical procedures and the hope is that this device could help patients avoid surgical intervention by aiding therapist during physical therapy. The project is being sponsored by Children’s Healthcare of Atlanta and the Atlantic Pediatric Device Consortium.
“The nice thing about mechanically assistive robotics is a therapist could use it to create new training paradigms for children with cerebral palsy to ultimately improve their long term clinical outcomes using these devices,” said Young.
Robotic Prosthesis
The robotic leg prosthesis is a two joint device, with powered knee and ankle joints. Most prosthetic legs are passive, using no power, and they are optimized for performing one task- walking on level surfaces. Young wanted to see what would happen if a device was designed to be able to adapt to a user’s needs, whether that’s climbing stairs, walking on a ramp, or moving around on flat ground. A major part of that is trying to understand when someone wants to transition between these different tasks and to be able to give the appropriate assistance at the right time. The goal is for it to be natural, automatic, and intuitive to the user with no need to hit buttons or switches during transitions. Instead the objective is to develop an intent recognition system that employs a variety of machine learning and artificial intelligence techniques to interpret sensor information and anticipate what the user is going to do next.
Autonomous Hip Exoskeleton
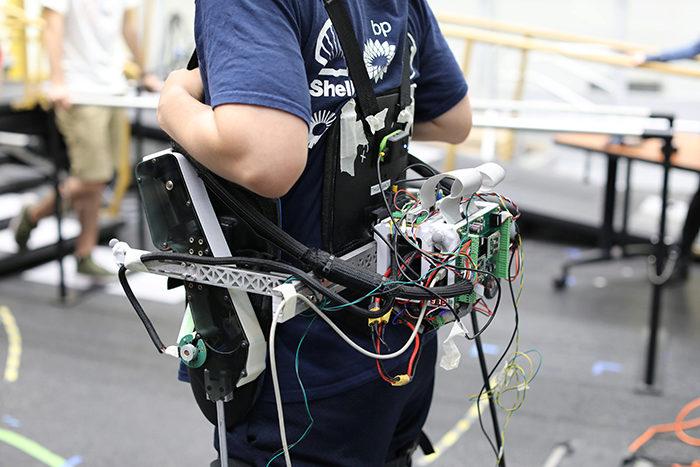
Designed primarily for stroke patients who have lost a degree of their mobility, the powered hip exoskeleton offers assistance in hip flexion and extension. Like the leg prosthesis, the amount of power need can fluctuate based on what the user is trying to do and whether they want to move faster or slower, up stairs, or down ramps. The device could be used to help users move around more comfortably and independently in their homes, or as a therapy device in a rehabilitation environment.
“The user may be able to walk but, they are not walking as well as they were before their injury,” said Young. “The ability to restore full community ambulation is really valuable for improving independence, quality of life, and overall happiness of any individual. Our focus is on trying to understand how to optimize the control interface so that it feels natural so the patient enjoys using it and is able to more easily get around through this augmented assistance.“
This project is being funded through the National Science Foundation (NSF) National Robotics Initiative and a National Institutes of Health (NIH) National Center for Medical Rehabilitation Research Young Investigator Award recently awarded to Young.

While the first three projects are focused on relatively narrow segments of the population with hopes of them being expanded down the road, an ankle exoskeleton is being developed for the aging population.
As Greg Sawicki describes it, the Achilles tendon is the powerhouse spring in the ankle, and as people age that spring loses its stiffness and subsequently loses its ability to store and return energy during a step. That results in more effort and energy being used by muscles to do the same amount of work that was once accomplished with vibrant tendon recoil. The ankle exoskeleton Sawicki’s team is developing uses a spring and clutch system to restore that bounce and compensate for the body’s natural decline, allowing people who have perhaps transitioned from the workforce into retirement to maintain active and independent lifestyles.
Although each of these projects is different there’s an underlying principle behind each of them that focuses on efficient mobility. The human body is an incredibly complicated machine, and as one part performs less than optimally other parts compensate, often to their detriment. For example, amputees often have higher rates of osteoarthritis and osteoporosis. There’s also the matter of fuel efficiency. Sawicki compares the body to a car- as parts wear out the efficiency of the vehicle declines, requiring more fuel to go the same distance. As an Achilles tendon loses its snap, leg muscles at the hip or knee must work harder, consuming more energy. By taking preventative steps through human augmentation with external, wearable robotics Sawicki and Young think they can help stave of decline in other parts of the body and extend the active and productive years of an aging population.
To accomplish all of this Young and Sawicki have a state of the art workspace staffed with interdisciplinary teams of postdocs, graduate students, and undergraduate researchers working together through Young’s Exoskeleton and Prosthetic Intelligent Controls (EPIC) lab and Sawicki’s Physiology of Wearable Robotics (PoWeR) lab to tackle the engineering, programming, and clinical challenges of restorativedevices. Truly interdisciplinary in nature, their research leverages the expertise and resources of a range of affiliations. Both Sawicki and Young belong to Georgia Tech’s Institute for Robotics and Intelligent Machines (IRIM) and are members of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory program faculty as well as members of Tech’s Parker H. Petit Institute for Bioengineering and Bioscience. Sawicki also has an appointment to Georgia Tech’s School of Biological Sciences. Those interdisciplinary connections allow the pair to attract students from across schools and majors.
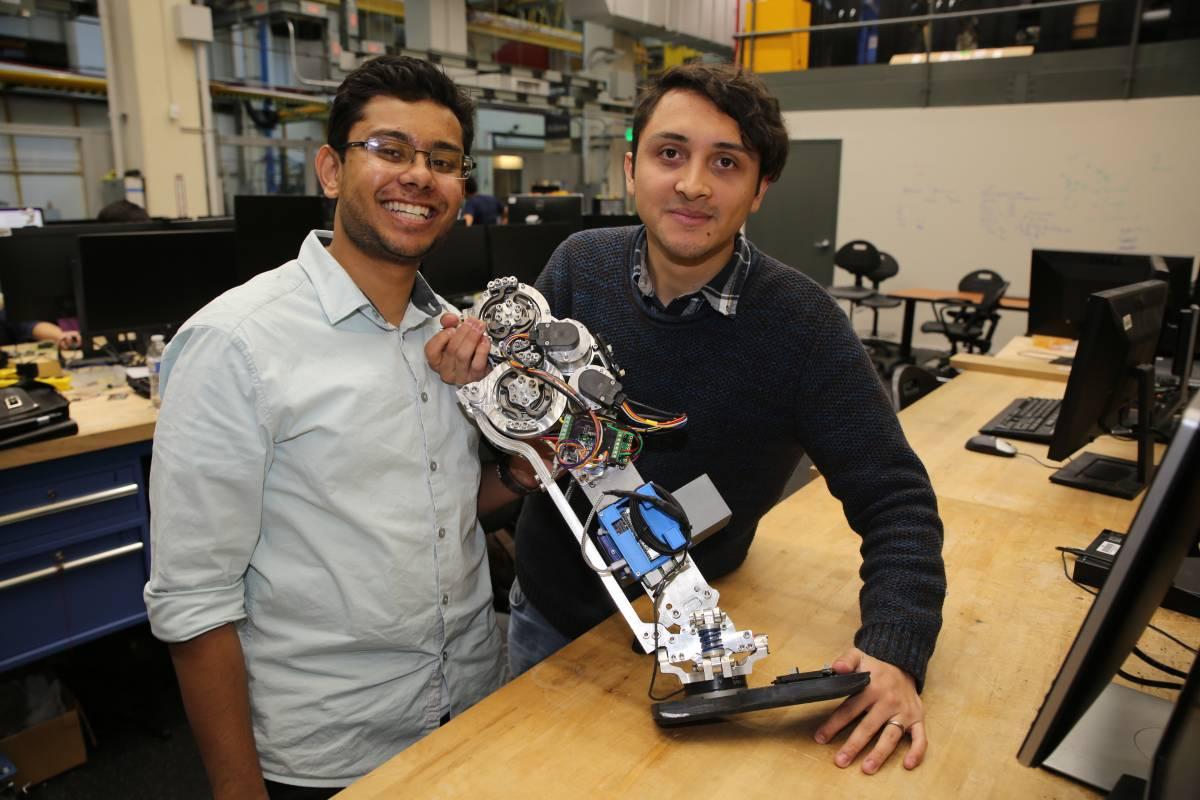
Mechanical engineers in the lab are focused on the design, fabrication, and refinement of the devices. Electrical and computer engineers develop the controls and wiring of the systems, and biomedical engineers look at how the devices interact with their users and help to understand the medical and biomechanical consequences of the projects. With a wide array of equipment that includes motion capture, muscle monitoring, and force plates throughout their labs that can capture, measure, and model the forces and consequences of every movement, team members can make sure that the exoskeletons and prostheses are functioning as intended and not adding extra strain to other parts of the body. The labs also include a team of computer scientists focused on developing the machine learning and artificial intelligence that serve as the foundation for the assistive technology.
On the clinical side, particularly with the lower limb prosthesis, the labs work with Georgia Tech’s master’s in prosthetics and orthotics (MSPO) program to find volunteers interested in helping to test the devices. The clinicians help to make sure the devices are properly aligned and safe to wear.
“The patients we recruit like being part of this,” says Kinsey Herrin, the clinical liaison and instructor in the Prosthetics and Orthotics program. “They like giving back and feeling like they're contributing to science. They enjoy the energy of it and being on the edge of something new.”
The collaboration between engineering, biology, computer science, and clinical medicine is one of the things that sold Aaron Young on coming to Georgia Tech as a faculty member.
“I think what is really unique about Georgia Tech is not only do you have the clinical resources of a large city with good supporting hospitals, but you have the really advanced research and engineering apparatus to partner with, especially on things like artificial intelligence, machine learning, and mechanical engineering. We have the capability to do design creation and prototyping on site and that really helps to set us apart from other places. As an incoming faculty member it's a place that's really attractive to do this kind of research where we can build everything at home, do a lot of good testing and implement lots of very interesting things. We have an amazing robotics community here, and that makes it a lot easier to do the interdisciplinary research that we're really trying to do.”
“I think we have one of the best facilities in the world now,” adds Sawicki. “We’re definitely one of the best in the nation for assessing how robots interact with people all the way from under the skin up through the whole body. We’re especially focused in this space on being able to understand how these things work out in the real world environment. It’s time to cross that hurdle now.”
This research was supported by grants to G.S.S. from the National Robotics Initiative via the National Institute of Nursing Research of the National Institutes of Health (R01NR014756), the National Institute on Aging of the National Institutes of Health (R01AG058615) and the U.S. Army Natick Soldier Research, Development and Engineering Center (W911QY18C0140).
This research was supported by grants to A.J.Y. from the NSF National Robotics Initiative (Award #1830215), the Office of the Assistant Secretary of Defense for Health Affairs through the Orthotics and Prosthetics Outcomes Research Program Prosthetics Outcomes Research Award under Award No. W81XWH-17-1-0031, and an NIH New Investigator NCMRR award (Grant Number: 1R03HD097740-01).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies listed.