Microsurgeon Shao-Yun Hsu takes treating her patients all the way to Georgia Tech, where she’s getting a Ph.D. and developing biomaterials to restore function — and quality of life — for people with lymphedema.
(text and background only visible when logged in)
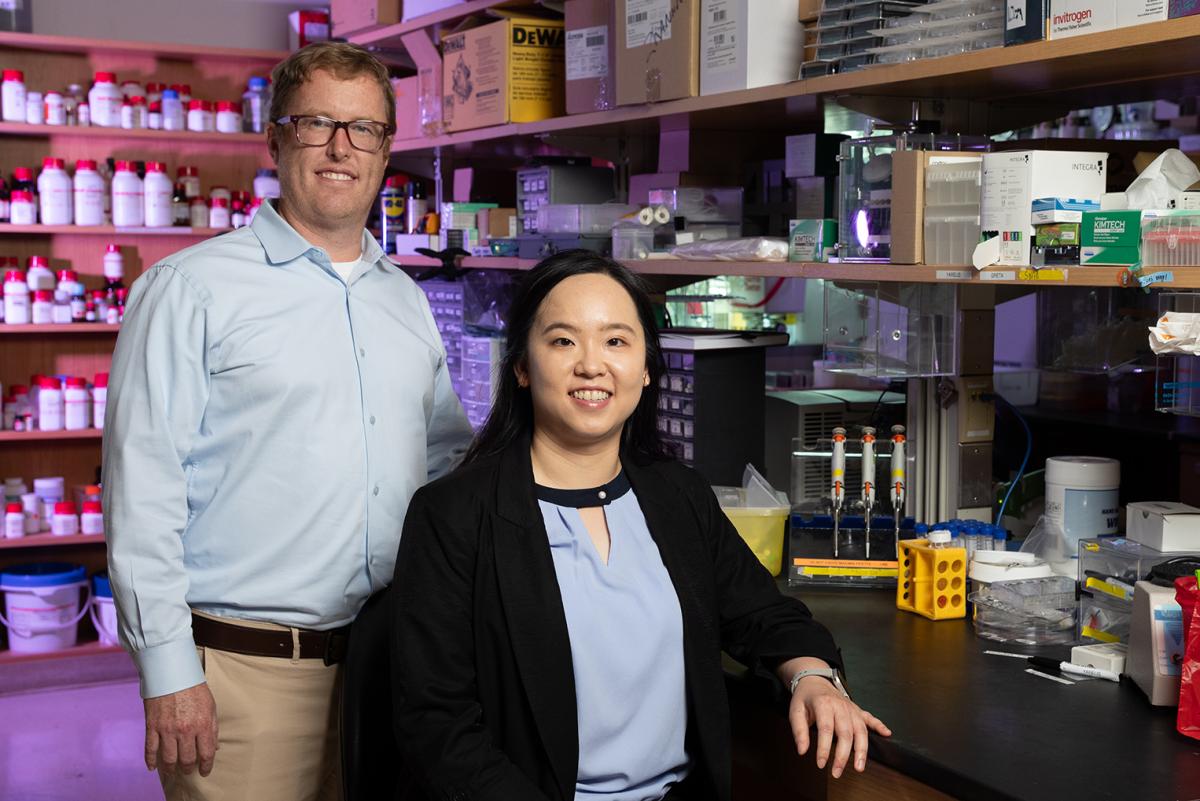
Brandon Dixon, left, and Shao-Yun Hsu are working to improve lymph node transplant surgery, a delicate procedure Hsu spent years training to perform as a microsurgeon in Taiwan. (Photo: Candler Hobbs)
Shao-Yun Hsu kept seeing the same name on research study after research study: Brandon Dixon, an engineer at Georgia Tech.
Hsu, a microsurgeon in Taiwan, was trying to figure out how to help her patients with lymphedema — an uncomfortable and life-limiting swelling in limbs that results from lymph nodes failing to drain fluid from an arm or leg.
Hsu had what she thought was a basic question: exactly how much fluid each small lymphatic vessel could drain. And as she dug into the clinical research, she saw Dixon’s name over and over.
Spoiler alert: There’s no good answer to Hsu’s question. At least not yet. But the search has brought her to Atlanta to pursue a biomedical engineering Ph.D. in Dixon’s lab.
Together, they’re embarking on a new project with support from the National Institutes of Health (NIH) that could one day help Hsu’s patients by making a lymph node transplant a viable option for many more people who suffer from lymphedema.
“Before I came to Georgia Tech, I had to transfer my patients to other physicians because lymphedema is a long-term disease, and I would no longer be around to treat them. Usually patients don’t like that,” said Hsu, who’s about halfway through her doctoral program. “But when I told them I was going to get my Ph.D. trying to find a new treatment for lymphedema patients, they gave me their best wishes. They put a lot of hope in me, telling me, ‘Go, but remember to come back, because we really need your help.’”
Lymphedema results from a disrupted or underdeveloped lymphatic system, resulting in fluid and fat accumulating in the affected arm or leg. More than 35 million Americans and 150 million people worldwide suffer from the condition.
Aside from the difficulty of using the now-deformed limb — which can grow by 50% or more in severe cases — lymphedema can be painful, compromise immune function, and cause repeated infections. It can result from breast cancer surgery, radiation therapy, and other conditions. There’s no cure.
A lymph node transplant is one possible treatment, but it only works for around a third of patients; figuring out who’s a good candidate is nearly impossible, Hsu said.
Engineers often collaborate with surgeons to solve difficult clinical problems like this. But Hsu’s interest presented a unique opportunity to have a highly trained surgeon right in the lab, Dixon said.
“You cannot teach a Ph.D. student to have the surgical skills of a microsurgeon with eight years of medical training and years of experience in the operating room,” said Dixon, Woodruff Professor in the George W. Woodruff School of Mechanical Engineering. “This was a once-in-a-lifetime opportunity for me to have a person who could do this human lymph node transplant surgery and adapt it for animal models.”
Two kinds of surgeries can potentially help lymphedema patients. Doctors can try to transplant lymph nodes from a different part of the patient’s body to restore function. Or they can connect damaged lymphatic vessels to nearby veins, which are larger and more flexible. The drained fluid is then filtered out of the circulatory system by the kidneys. They’re performed more often in Taiwan and Japan, for example, than the United States. Neither is a guaranteed success.

That’s where Hsu and Dixon’s new NIH project comes in. They’re working with Georgia Tech colleague Andrés García and collaborators at Yale to increase the odds for patients by supercharging lymph node transplant procedures.
They’ll transplant lymph nodes and deploy an engineered biomaterial called a hydrogel that Dixon developed with García. They’ll also use tiny fat bubbles called lipid nanoparticles to deliver a growth factor to the surrounding lymphatic system.
The idea is to reconnect the transplanted nodes and restore proper fluid flow.
“We have two big goals,” Dixon said. “One is to improve the efficacy of lymph node transplant to where it works in more than 30% of patients. The second, and maybe more ambitious goal, is that perhaps the lymph node transplant itself is not necessary. If we can replace the entire lymph node with a hydrogel — once we really understand what it's doing when it regrows — perhaps you don't need to be a microsurgeon now.”
Hsu came to Georgia Tech trying to understand how much fluid is drained by each lymphatic vessel so she and her fellow doctors could find the ideal rerouting approach to help patients. Now she’s broadened her view, working to perhaps replace the lymph node transplant surgery that she trained for years to do.
It doesn’t seem to bother her. One of her surgical mentors always told her that’s exactly what top surgeons should do. Plus, she keeps thinking about her patients.
“One of my patients had a full recovery after lymph node transfer surgery. He was lucky. He showed me a photo from before treatment where he was only able to lie down at home because his leg was so heavy. Two years after surgery, he climbed the highest mountain in Taiwan,” Hsu said.
“If this works, it can change a lot of lives.”
(text and background only visible when logged in)
Related Content

Nanotechnology Approach Shows Promise for Treating Lymphedema
ME researchers Brandon Dixon and Susan Thomas use nanoparticles to deliver a drug therapy directly to lymph vessels and restore their fluid-draining function.
ME researchers Brandon Dixon and Susan Thomas use nanoparticles to deliver a drug therapy directly to lymph vessels and restore their fluid-draining function.
Cancer Fighters
Engineers are rewiring cells and creating new tools to improve cancer therapies and catch the disease earlier.
Engineers are rewiring cells and creating new tools to improve cancer therapies and catch the disease earlier.