Story by Kathleen Moore
Photographs by Gary Meek and Kathleen Moore
Wassim Haddad will be the first to tell you that he’s no businessman. The author of numerous books and papers on subjects ranging from mathematics and philosophy to dynamical systems and thermodynamics, he is a scholar first and foremost.
But when his interest in dynamical system modeling and control led him repeatedly into the realm of pharmacology and neuroscience, the aerospace engineering professor could not ignore the obvious. That’s how AreteX Engineering was born.
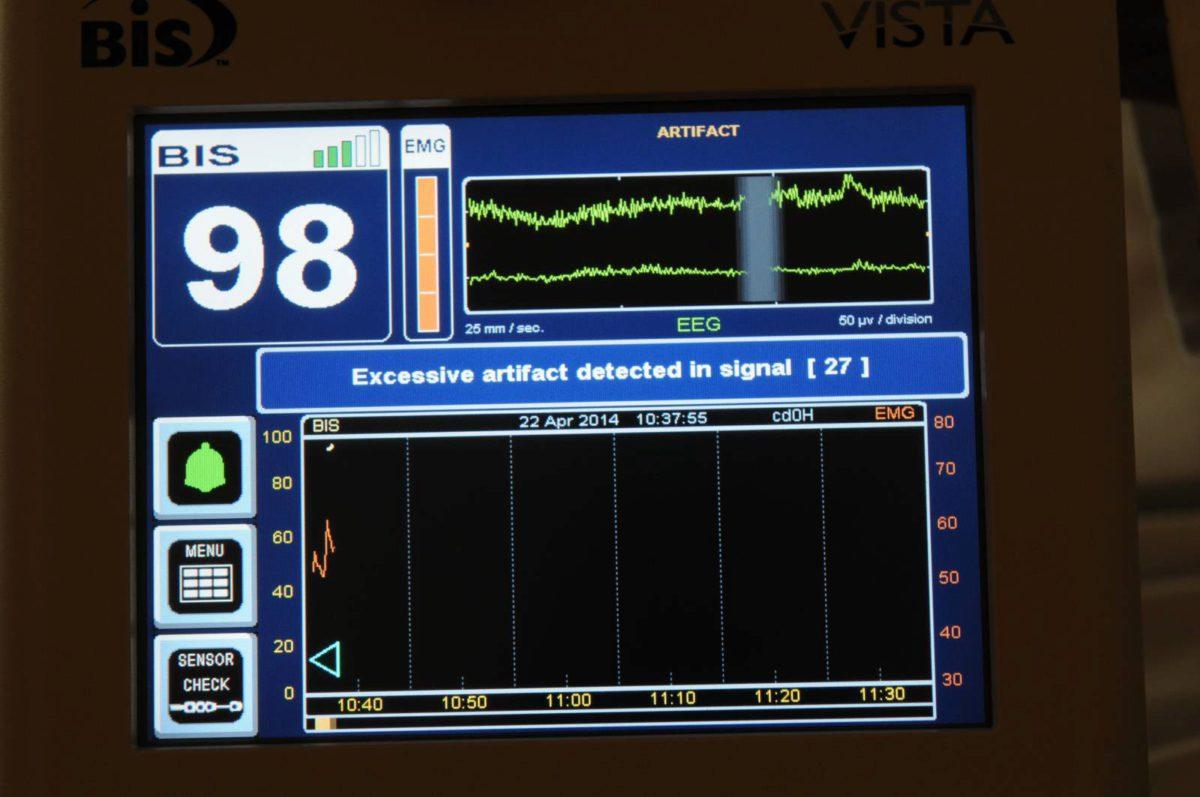
Launched in 2012, the NYC-based company is developing a technology that could eliminate over- and under-sedation, a problem that currently affects thousands of hospital and nursing facility patients each year. Already studied in surgical settings, the AreteX technology seeks to improve anesthesia delivery by drawing upon an expanded database of behavioral and physiological indices to guide dosage levels.
The research – and the philosophy – behind it have been building critical mass in Haddad’s mind for more than a decade. He is excited that they are both, now, coming together.
“I have always maintained that there are many connections between thermodynamics – the science of large-scale dynamical systems with interconnected components or parts that exchange energy and matter among subsystems – and neuroscience,” he says.
“I realized that with a suitable reinterpretation of system variables in one discipline, we can transition and develop new theories in another to solve pressing problems,” he continues.
“And that’s what we are doing with AreteX. We are using machine learning, Bayesian networks, and dynamical system modeling to assess sedation and pain levels as well understand patient outcomes in the ICU.”
In addition to receiving startup grants from the National Science Foundation and the U.S. Army Medical Research and Material Command, AreteX is currently in talks with the NYU Langone Medical Center to begin clinical trials on a new suite of technology and protocols that will use physiological and behavioral data to more precisely calibrate patient drug dosages in the ICU. With a more robust database, the system better addresses sedation and pain management. The company started a pilot study at the Northeast Georgia Medical Center (NGMC) earlier this year.
Another grant, currently in the works, could bring AreteX’s prototype to market within a year.
Haddad is joined in this venture by his longtime research partner Dr. James Bailey, an NGMC anesthesiologist, and Dr. Behnood Gholami, a former AE doctoral student of Haddad’s who went on to do post-doctoral research at Harvard Medical School.
“We are introducing a series of multi-modal sensors to this process so that clinicians will be able to base patient care on behavioral and physiological measurements,” said Bailey. “If we can remove the subjectivity, we will be able to better use the knowledge and judgment of our medical staffs.”
The problem with general anesthesia
As many as 2 percent of all surgical patients have been found to be insufficiently anesthetized, a condition that permits them to be fully aware during an operation but unable to inform their surgeon because they are paralyzed.
“That may not sound like a high percentage but, when you consider that there over 20 million surgical procedures conducted in the United States each year, the numbers are compelling,” said Haddad. “It is a nightmare when things go wrong.”
The problem is less traumatic but more pronounced in the nation’s ICUs, where as many as 70 percent of the patients who receive sedation are either under or over-sedated, Haddad noted.
The results of under-sedation – patient trauma, excessive movement, unnecessary pain, the accidental removal of life-support equipment – can delay patient diagnosis, prolong hospital stays, and require additional interventions. Haddad estimates that this costs the U.S. healthcare system upwards of $400 million annually.
Over-sedated patients are spared from excessive pain, trauma or muscle movement but may be harder to wean from mechanical ventilators and more likely to remain hospitalized longer. Haddad estimates that more than $4 billion could be saved annually if the average use of mechanical ventilators in ICUs was reduced by just one day.
“The problem — in the ICU and in the operating room — is that there’s no consensus on the definition of adequate sedation,” says Bailey (above).
“If there is a question as to whether a patient needs additional sedation, the common practice is to give more, to be on the safe side. But there is no clinical evidence that this is needed, and the process itself puts an undue burden on medical staff, particularly ICU nurses, who have to do everything from bathing and feeding patients to drug titration.”
Lessons learned from airplanes and algorithms
If AreteX Engineering has its way, this imprecision will soon be a thing of the past.
“What we are doing for anesthesia is, essentially, what the auto-pilot did for airplanes,” says Haddad.
“You would not want an airline pilot to spend all of his time manning the controls of an airplane. And you do not want an anesthesiologist to spend all of his time interpreting numerous sensors and manually titrating patient anesthetic drug doses. He should be alert and able to intervene in emergencies, not taxed by routine data interpretation. Manual control can be very tedious, imprecise, time consuming, and sometimes of poor quality.”
Into this scenario, Haddad and AreteX are introducing a closed-loop controller for intraoperative anesthesia and a clinical decision support system (CDSS) to better manage sedation and pain.
The CDSS simultaneously collects a large array of behavioral and physiological data on each patient, which it feeds into a machine learning algorithm — an algorithm that determines the probability of patient pain and sedation levels.
Ultimately, in a closed-loop system, this data will be fed into an actuator (for example, an infusion pump) that will automatically administer the right levels of medicine directly to the patient. Right now, the machine’s recommendations are provided to the clinician for improving sedation management manually.
“Closed-loop control is superior to open-loop [manual] control because it allows you to maintain sedation at targeted levels throughout, rather than having to constantly correct drug dosage as the patient metabolizes the drugs,” says Bailey, who has overseen more than 50 clinical trials of a similar system in the operating rooms at Emory University Hospital and the NGMC.
“My gut impression is that the closed-loop controller does as well as I do – maybe even a little better. Overall, it has tended to require a little less anesthesia. We know when to administer it and how much is needed. And we had no instances of patients waking up or having any adverse effects.”
Bailey’s faith in this system is not based solely on personal experience or gut impressions, however. Data is king. And the AreteX CDSS system collects a lot of it. Among the primary sensors for assessing pain and sedation levels:
• Electrocardiograph to detect pulse and heart rate variability;
• Electroencephalograph to determine brain activity, particularly parameters that indicate awareness; and
• Digital imaging that captures behavioral data, such as patient movement, which indicate pain or awareness.
“Any one of these indicators, alone, can lead to a misleading assertion, but, when basing our assessment on multi-modal sensor measurements, that minimizes the chance of assessment error,” says Gholami. “We have developed performance measures [for all of these indicators] that support more accurate interpretation and decision support for sedation management.”
That said, there is no one-size-fits all interpretation when it comes to patient care. The AreteX CDSS will take this into account.
“The closed-loop controller that we developed for intraoperative anesthesia is adaptive, which means the patient parameters can change every time you hook it up to a different patient,” said Haddad.
The parameters of a 98-pound female runner will be very different from those of an overweight diabetic male patient. The control system accounts for that. It senses a different level of brain activity and takes information from all sensors to determine the amount of drug needed.
Right now, Haddad, Bailey and Gholami are targeting the CDSS for deployment in ICUs, where anesthesia is routinely used to manage millions of patients who are hooked up to ventilators and other rehabilitative equipment. But they have also set their sights on the nation’s operating rooms, where anesthesiologists regularly oversee operations that can last eight to12 hours or more.
“And sometimes, they are coming into those surgeries after having just completed another one,” Haddad says. “Imagine how much this control technology could improve the accuracy and quality of anesthesia administration which forms the foundation of almost all surgeries.”
Ed. note: This story appears in the Summer/Fall 2014 issue of Georgia Tech Engineers, the magazine from the College of Engineering. To request a copy, please email the editor at editor@coe.gatech.edu